Skin Cancer Care
Services • Dermatology Associates of Oak Ridge, P.C.
Skin cancer is the most common form of human cancers, affecting more than one million Americans every year. One in five Americans will develop skin cancer at some point in their lives. Skin cancers are generally curable if caught early. However, people who have had skin cancer are at a higher risk of developing a new skin cancer, which is why regular self-examination and doctor visits are imperative.
The vast majority of skin cancers are composed of three different types: basal cell carcinoma, squamous cell carcinoma and melanoma.
With any kind of with any skin cancer, the treatment options available to a patient depend on the tumor type, size, location and depth, plus age and overall health. Learn more about treatment options below.
Basal Cell Carcinoma
This is the most common form of skin cancer. Basal cells reside in the deepest layer of the epidermis, along with hair follicles and sweat ducts. When a person is overexposed to UVB radiation, it damages the body's natural repair system, which causes basal cell carcinomas to grow. These tend to be slow-growing tumors and rarely metastasize (spread).
Basal cell carcinomas can present in a number of different ways:
- Raised pink or pearly white bump with a pearly edge and small, visible blood vessels
- Pigmented bumps that look like moles with a pearly edge
- A sore that continuously heals and re-opens
- Flat scaly scar with a waxy appearance and blurred edges

Despite the different appearances of the cancer, they all tend to bleed with little or no cause. Eighty-five percent of basal cell carcinomas occur on the face and neck since these are areas that are most exposed to the sun.
Risk factors for basal cell carcinoma include having fair skin, sun exposure, age (most skin cancers occur after age 50), exposure to ultraviolet radiation (as in tanning beds) and therapeutic radiation given to treat an unrelated health issue.
Diagnosing basal cell carcinoma requires a biopsy — either excisional, where the entire tumor is removed along with some of the surrounding tissue, or incisional, where only a part of the tumor is removed (used primarily for large lesions).
Treatments for basal cell carcinoma include:
- Curettage and Desiccation — The preferred method of dermatologists, this treatment involves using a small metal instrument (called a curette) to scrape out the tumor along with an application of an electric current into the tissue to kill off any remaining cancer cells.
- Mohs Micrographic Surgery — The preferred method for large tumors, Mohs Micrographic Surgery combines removal of cancerous tissue with microscopic review while the surgery takes place. By mapping the diseased tissue layer by layer, less healthy skin is damaged when removing the tumor.
- Surgical Excision — In this treatment, the tumor is surgically removed and stitched up.
- Radiation Therapy — Radiation therapy is used for difficult-to-treat tumors, either because of their location, severity or persistence.
- Cryosurgery — Some basal cell carcinomas respond to cryosurgery, where liquid nitrogen is used to freeze off the tumor.
- Prescription Medicated Creams — These creams can be applied at home. They stimulate the body's natural immune system over the course of weeks.
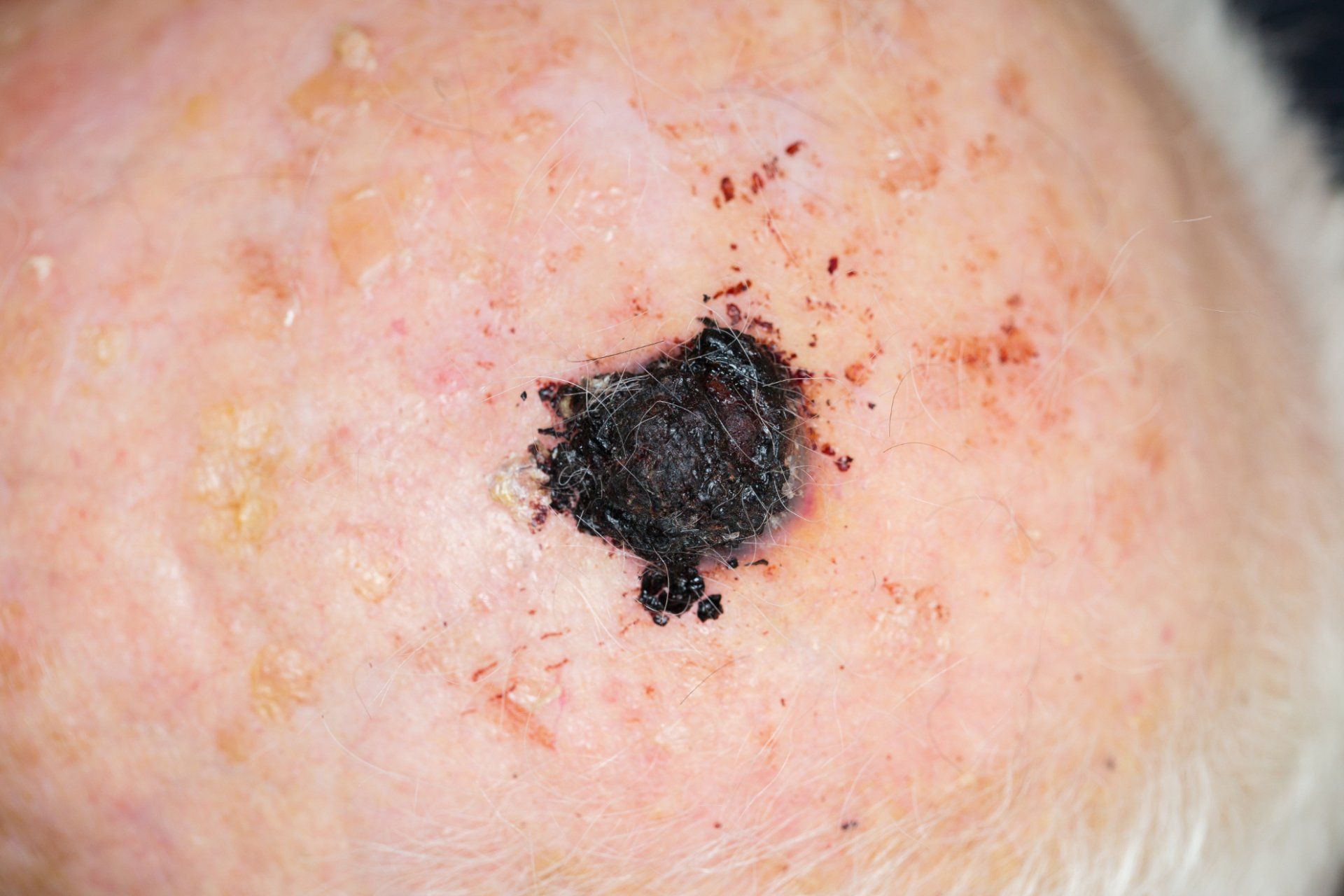
Squamous Cell Carcinoma
Squamous cells are found in the upper layer (the surface) of the epidermis. They look like fish scales under a microscope and present as a crusted or scaly patch of skin with an inflamed, red base. They are often tender to the touch. It is estimated that 250,000 new cases of squamous cell carcinoma are diagnosed annually, and that 2,500 of them result in death.

Squamous cell carcinoma can develop anywhere, including inside the mouth and on the genitalia. It most frequently appears on the scalp, face, ears and back of hands. Squamous cell carcinoma tends to develop among fair-skinned, middle-aged and elderly people who have a history of sun exposure. In some cases, it evolves from actinic keratoses, dry scaly lesions that can be flesh-colored, reddish-brown or yellow black, and which appear on skin that is rough or leathery. Actinic keratoses spots are considered to be precancerous.
Like basal cell carcinoma, squamous cell carcinoma is diagnosed via a biopsy — either excisional, where the entire tumor is removed along with some of the surrounding tissue, or incisional, where only a part of the tumor is removed (used primarily for large lesions).
Treatments for basal cell carcinoma include:
- Surgical Excision — In this treatment, the tumor is surgically removed and stitched up.
- Mohs Micrographic Surgery — The preferred method for large tumors, Mohs Micrographic Surgery combines removal of cancerous tissue with microscopic review while the surgery takes place. By mapping the diseased tissue layer by layer, less healthy skin is damaged when removing the tumor.
- Curettage and Desiccation — The preferred method of dermatologists, this treatment involves using a small metal instrument (called a curette) to scrape out the tumor along with an application of an electric current into the tissue to kill off any remaining cancer cells.
- Radiation Therapy — Radiation therapy is used for difficult-to-treat tumors, either because of their location, severity or persistence.
- Cryosurgery — Some basal cell carcinomas respond to cryosurgery, where liquid nitrogen is used to freeze off the tumor.
- Prescription Medicated Creams — These creams can be applied at home. They stimulate the body's natural immune system over the course of weeks.
Melanoma
While melanoma is the least common type of skin cancer, it is by far the most virulent. It is the most common form of cancer among young adults age 25 to 29. Melanocytes are cells found in the bottom layer of the epidermis. These cells produce melanin, the substance responsible for skin pigmentation. That's why melanomas often present as dark brown or black spots on the skin. Melanomas spread rapidly to internal organs and the lymph system, making them quite dangerous. Early detection is critical for curing this skin cancer.
Melanomas look like moles and often do grow inside existing moles. That's why it is important for people to conduct regular self-examinations of their skin in order to detect any potential skin cancer early, when it is treatable. Most melanomas are caused by overexposure to the sun beginning in childhood. This cancer also runs in families.
Melanoma is diagnosed via a biopsy. Treatments include surgical removal, radiation therapy or chemotherapy.
What to Look For
The key to detecting skin cancers is to notice changes in your skin. Look for:
- Large brown spots with darker speckles located anywhere on the body.
- Dark lesions on the palms of the hands and soles of the feet, fingertips toes, mouth, nose or genitalia.
- Translucent pearly and dome-shaped growths.
- Existing moles that begin to grow, itch or bleed.
- Brown or black streaks under the nails.
- A sore that repeatedly heals and re-opens.
- Clusters of slow-growing scaly lesions that are pink or red.

The American Academy of Dermatology has developed the following ABCDE guide for assessing whether or not a mole or other lesion may be becoming cancerous.
- Asymmetry: Half the mole does not match the other half in size, shape or color.
- Border: The edges of moles are irregular, scalloped, or poorly defined.
- Color: The mole is not the same color throughout.
- Diameter: The mole is usually greater than 6 millimeters when diagnosed, but may also be smaller.
- Evolving: A mole or skin lesion that is different from the rest, or changes in size, shape, or color.
If any of these conditions occur, please
make an appointment to see one of our
dermatologists right away. The doctor may do a biopsy of the mole to determine if it is or isn't cancerous.
Prevention
Roughly 90% of nonmelanoma cancers are attributable to ultraviolet radiation from the sun. That's why prevention involves:
- Staying out of the sun during peak hours (between 10 a.m. and 4 p.m.).
- Covering up the arms and legs with protective clothing.
- Wearing a wide-brimmed hat and sunglasses.
- Using sunscreens year round with a SPF of 15 or greater and sunblocks that work on both UVA and UVB rays. Look for products that use the term "broad spectrum."
- Checking your skin monthly and contacting your dermatologist if you notice any changes.
- Getting regular skin examinations. It is advised that adults over 40 get an annual exam with a dermatologist.

Mohs Micrographic Surgery
Highly Effective Skin Cancer Treatment Performed by a Board-Certified Dermatologist and Fellowship-Trained Mohs Surgeon
The preferred method for large tumors, Mohs Micrographic Surgery combines removal of cancerous tissue with microscopic review while the surgery takes place. By mapping the diseased tissue layer by layer, less healthy skin is damaged when removing the tumor.
Our Mohs specialist, Katherine Kerchner M.D., FAAD, is a Fellowship-Trained Mohs Surgeon, who has more experience with Mohs Surgery than other specialists in the area.
Curious if Mohs is the right fit for you? Call us at 865-482-2129 today to schedule a consultation.